 |
|
|
|
Are Face Masks of N-95 Quality Imperative To Mitigate Infection? The internationally respected Lancet publication reported in April 2021, on the evidence that Covid-19 (SARS-CoV-2 ) is airborne and spreads from room to room and infects people via the air they breathe, and NOT just as a result of close contact with someone infected or carrying the disease. “There is consistent, strong evidence that SARS-CoV-2 spreads by airborne transmission. Although other routes can contribute, we believe that the airborne route is likely to be dominant. The public health community should act accordingly and without further delay.” – conclusion of the Lancet Article. The article based upon research conducted on behalf of the World Health Organisation (WHO) introduces this stalk warning for public health:
Airborne transmission of respiratory viruses is difficult to demonstrate directly. Mixed findings from studies that seek to detect viable pathogen in air are therefore insufficient grounds for concluding that a pathogen is not airborne if the totality of scientific evidence indicates otherwise. Decades of painstaking research, which did not include capturing live pathogens in the air, showed that diseases once considered to be spread by droplets are airborne." The Lancet gives 10 reasons which prove that Covid is airborne: 1 Superspreading events account for substantial SARS-CoV-2 transmission; indeed, such events may be the pandemic's primary drivers. Detailed analyses of human behaviours and interactions, room sizes, ventilation, and other variables in choir concerts, cruise ships, stadia based events, care homes, and prisons, among other settings, have shown long-range transmission that cannot be adequately explained by droplets or fomites. 2 Long-range transmission of SARS-CoV-2 between people in adjacent rooms but never in each other's presence has been documented in quarantine hotels. 3 Asymptomatic or presymptomatic transmission of SARS-CoV-2 from people who are not coughing or sneezing is likely to account for at least a third, and perhaps up to 59%, of all transmission globally and is a key way SARS-CoV-2 has spread around the world, 4 Transmission of SARS-CoV-2 is higher indoors than outdoors and is substantially reduced by indoor ventilation.Both observations support a predominantly airborne route of transmission.
6 Viable SARS-CoV-2 has been detected in the air. In laboratory experiments, SARS-CoV-2 stayed infectious in the air for up to 3hrs with a half-life of 1·1hrs. Viable SARS-CoV-2 was identified in air samples from rooms occupied by COVID-19 patients in the absence of aerosol-generating health-care procedures and in air samples from an infected person's car. 7 SARS-CoV-2 has been identified in air filters and building ducts in hospitals with COVID-19 patients; such locations could be reached only by aerosols. 8 Studies involving infected caged animals that were connected to separately caged uninfected animals via an air duct have shown transmission of SARS-CoV-2 that can be adequately explained only by aerosols. 9 No study to our knowledge has provided strong or consistent evidence to refute the hypothesis of airborne SARS-CoV-2 transmission. 10 There is limited evidence to support other dominant routes of transmission—ie, respiratory droplet or fomite.
Ease of infection between people in close proximity to each other has been cited as proof of respiratory droplet transmission of SARS-CoV-2. However, close-proximity transmission in most cases along with distant infection for a few when sharing air is more likely to be explained by dilution of exhaled aerosols with distance from an infected person. You can read and download the full Lancet article from the Lancet website here
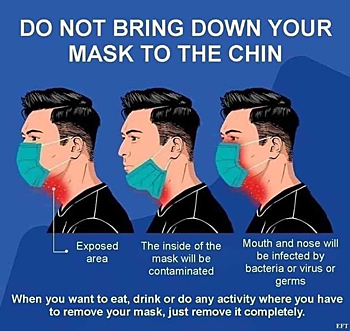
Further on reading the article in its entirety, it becomes clear that test and trace has failed not only because the system doesn’t actually work and follow-up of those testing positive and their contacts; has been patchy to say the least according to a variety of media sources; but because of the method used to take samples and the testing methodology. It also explains, in part, why the current ‘lateral flow tests’ are so unreliable, as concluded by Liverpool University and others following study of the pilot test and trace sites in Liverpool using this type of testing regime. With concerns over the mutation of the virus, and particularly of the Indian variation now found in Bolton in the North West of England; the Government are going to have to take evidence such as this from the Lancet and modify their current actions and policies. Many in the scientific, public health, and medical communities, believe that a third wave as experienced in countries who were further ahead than the UK in preventive actions and treatments and had a much lower fatality count; is inevitable given the UK population behaviours, incorrect use of face masks and the generally flimsiness of them, along with the anti-vaccination lobby on social media. Source: The Lancet / Unionsafety
|


 5 Nosocomial infections (health-care-associated or hospital-acquired infections) have been documented in health-care organisations, where there have been strict contact-and-droplet precautions and use of personal protective equipment (PPE) designed to protect against droplet but not aerosol exposure.
5 Nosocomial infections (health-care-associated or hospital-acquired infections) have been documented in health-care organisations, where there have been strict contact-and-droplet precautions and use of personal protective equipment (PPE) designed to protect against droplet but not aerosol exposure. This evidence and conclusion is such that our current Government and advisers are ignoring, because it does not fit in with their policy and aims.
This evidence and conclusion is such that our current Government and advisers are ignoring, because it does not fit in with their policy and aims.